“What does the G-I system have to do with autism?” The short answer is that it is often associated with behaviors of ASD, and so it needs to be addressed. What if diagnosing intestinal problems and improving gut health in non-verbal children did NOTHING ELSE other than assist in improving their overall well-being? How can anyone find fault with that strategy?
The longer answer is that there is a great deal of scientific evidence documenting a gut-brain connection in everyone, not just autistic patients. Eat an especially greasy meal and tell me you want to learn new skills. After ingesting some un-yummy fare, aren’t you grouchy? Are you ready to sit still and focus on new activities? When you get hungry, don’t you have trouble concentrating? “Butterflies in your stomach” before an anxious moment?
Dr. Michael Gershon of Columbia-Presbyterian University has published about this subject for over 40 years. “Our research is focused on the enteric nervous system (ENS), the intrinsic innervation of the bowel. This is the only part of the peripheral nervous system that is capable of mediating reflex behavior in the absence of input from the brain or spinal cord.”
Why is it so difficult for modern medical personnel to accept this concept? Perhaps because it sounds weird, unscientific, simplistic, and you can’t really SEE that system? Even today, the gut-brain connection remains a topic of debate.
However, once it becomes clear that there is a connection, it becomes easier to envision how important it would be for a sick child to get the best diagnosis and treatment for a “belly ache”.
Autistic children may never complain about pain. We often observe ‘gut behaviors’ where the patient lies on the floor on their stomach and ‘swims’ or frequently bends over a table. They deserve our investigation. Experience has shown that recognizing and addressing this connection is key to reducing mental “fog,” improving language acquisition, and minimizing disruptive activities.
A frequent finding in young children with self-injurious behavior is intestinal inflammation due to:
- Parasites
- Yeast – Fungus – Mold
- Pathogenic (harmful) Bacteria
- Other Toxins, including Heavy Metals
And PICA – the act of eating things that are NOT FOOD – increases when these disturbances exist. That can lead to a vicious cycle and more challenging behaviors. Accurate diagnosis helps identify safe and effective interventions; such as anti-parasitic, anti-fungal, specific probiotics (healthy bacteria), and detoxification supplements that produce measurable outcomes, .
I often relate to parents that the reason why their child appears to have “ants in their pants” is sometimes because they have ants in their pants!
So, if we can agree that there is a close relationship between G-I status and state-of-mind, and that non-verbal patients deserve consideration of a problem in that axis, why would it be so impossible to believe that some diets in some patients may prove worthwhile? The well-publicized University of Rochester study claiming “Popular Autism Diet Does Not Demonstrate Behavioral Improvement” specifically excluded “allergic” patients and was only able to enforce the diet on a handful of children for a month. Does that make all the other families who have instituted such a diet and seen real improvements in their child somehow irrelevant or incorrect?
Administering a special diet often makes the parents seem like “kooks”. Anyone who understands the time and patience that it takes to raise an ASD-affected child knows that the primary caretaker is perfectly aware of when things are going better. Which exact diet, what kinds of foods that are restricted or included, and the tests that assess food sensitivities are measurable to some extent, and practitioners can monitor the frequency, severity, and duration of offensive behaviors within that framework.
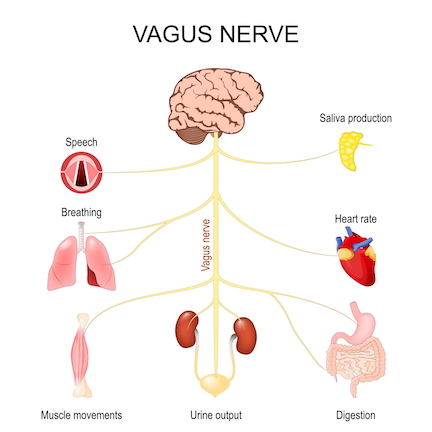
Adjustments to the spine around the 10th cranial nerve (vagus nerve) when there is inflammation or mis-alignment may explain the behavioral and cognitive improvements often observed following chiropractic manipulation. Additionally, hands-on practices, such as Neuromuscular Reflex Integration (NMRI) can provide avenues to this gut-brain-developmental axis, through which many families have noted improvements. Skilled occupational, physical and behavioral therapists, likewise, continue to observe results in an other-than-the-intended target when properly addressing the muscular tone and motor apraxia experienced by affected patients.
“More research” is always sought after to offer interventions and to document clinical significance. In the meantime, a better understanding of this important whole body relationship connecting the brain in the skull and our ‘2nd brain‘ in our digestive system will go a long way in understanding the observed behaviors of autism spectrum disorder by providing a choice of safe treatments that may contribute to improved outcomes.





Hello Dr Udell. Does it mean that heavy metals, molds, parasites in ASD people are caused by the disfunction between the gut and NS ? Is the disfunction caused by b 12 or folate deficiency in some cases?
Causes and effects in this protocol are less critical than clinical response. The improvements observed by mB12, leucovorin are apparent WHETHER OR NOT the patient has metals, deficiency, blocking/binding antibodies, MTHFR variations, etc!